In the case of chronic kidney failure, also known as chronic renal insufficiency or weakness, the function of the kidneys decreases over months or years. In contrast to the chronic form, acute kidney failure develops quickly, often within hours.
Chronic kidney failure often occurs as a result of diabetes mellitus, high blood pressure, inflammation of the kidneys, use of certain medications or as a result of hereditary malformations. Initially, the disease almost never causes symptoms. Then the appetite is often the first to decrease, and physical and mental performance decreases. Itching, pain, cardiac arrhythmias, nausea, vomiting and, in extreme cases, life-threatening urinary poisoning are possible later.
In early stages, therapies can slow the premature deterioration of the disease. In the final stage, only renal replacement therapies such as dialysis and transplantation can help. Chronic kidney failure reduces life expectancy.
 |
| Chronic kidney failure |
Causes, risk factors and frequency
Many causes of chronic kidney failure are already listed under "Causal treatment". In recent decades, the number of diseases as a result of diabetes mellitus and high blood pressure has risen particularly sharply. According to statistics, the most common causes are distributed roughly as follows:
- 30% of diseases are caused by diabetes mellitus
- 20% from high blood pressure
- 12 to 20% from kidney infections such as glomerulonephritis and interstitial nephritis
- 8 to 10% from drugs, especially painkillers
- 5% due to hereditary kidney diseases such as cystic kidneys
Risk factors
The risk factors largely correspond to the causes. So it's mostly about
- Acquired diseases (e.g. type 2 diabetes mellitus, high blood pressure, arteriosclerosis, kidney inflammation),
- Hereditary diseases (e.g. cystic kidneys),
- Treatments with drugs that can be harmful to the kidneys (e.g. painkillers, antibiotics, blood pressure, contrast agents).
Frequency
Chronic kidney failure is particularly common among people over the age of 80. Before the age of 50 it is very rare. The frequency increases with age.
According to surveys, an average of 7 out of 100 people in industrialized nations have impaired kidney function. The number of cases is increasing.
Symptoms
Do you often feel tired, have trouble concentrating and have trouble remembering things?
Do you often lack the appetite to eat with pleasure?
Maybe your legs are swollen and short of breath?
These can be signs of chronic kidney failure - but they don't have to be: kidney failure rarely causes symptoms in the early stages. Those affected can even notice nothing of their disease up to stage 4.
In the later course, substances accumulate in the blood and organs that healthy people normally excrete with the urine. These urinary substances mess up the electrolyte balance, the acid-base balance and many other processes. In addition, the hormone production of the kidneys is disrupted. The symptoms of chronic kidney failure can be varied. Those affected may have these symptoms:
- Tiredness, exhaustion, reduced physical performance
- Poor concentration, confusion, reduced mental performance
- Loss of appetite, nausea, vomiting, diarrhea
- Edema (fluid retention) e.g. in legs, face, lungs
- Shortness of breath, cardiac arrhythmia, heart failure
- Increased susceptibility to infections
- Elevated blood pressure (hypertension)
- Slowly decreasing amount of urine, possibly after an initially short increase
- Headache
- Itching all over the body
- Changed skin color - pale, gray or yellow-brown
- Erectile dysfunction, impotence
- "Restless legs" when falling asleep (technical term: restless legs syndrome)
- Bone pain, increased tendency to break bones
Tests may show values that deviate from the normal state and that can be associated with noticeable symptoms:
- Anemia (technical term: anemia)
- Disturbances in the water, electrolyte and acid-base balance
- Decreased excretion of drugs
- Degradation of the bone substance
Chronic kidney failure significantly increases the risk of serious cardiovascular disease. Most of those affected die of heart failure, heart attack and stroke. It is therefore important to keep an eye on your own kidney values, especially if risk factors for chronic kidney failure are present.
People with diabetes mellitus or high blood pressure should have regular blood and urine tests to monitor kidney function. The diseases are the most common causes of chronic kidney failure.
Many texts use "chronic renal failure" and "chronic renal failure" largely synonymously. "Insufficiency" means inadequacy or weakness - that something works worse than it should. It doesn't matter whether the loss is small or large. Nevertheless, some experts first speak of "insufficiency" and only then of "failure" when the kidney function largely or completely fails.
Treatment
After an initial consultation, doctors usually feel and tap the kidney area. They also look for edema and other abnormalities.
Ultrasound examinations of the kidneys and the rest of the urinary tract together with laboratory tests provide information on the form, severity and possible causes of kidney weakness.
To determine how well the kidneys are working, several tests are usually carried out. Important values are the glomerular filtration rate (GFR), the creatinine level and the creatinine clearance (see below).
In the case of unclear results, a suspicion of certain causes and consequential damage, further imaging procedures can be useful (e.g. X-ray, Doppler sonography, computed tomography, angiography). In some cases, only tissue removal (technical term: biopsies) from the kidneys allow a reliable diagnosis.
Once the reason for chronic kidney failure has been identified, medical therapy is aimed specifically at the cause. In later stages, therapies against complications and secondary diseases come more to the fore.
In addition, those affected should change their lifestyle so that the disease progresses as slowly as possible.
Control examinations and measurements are usually carried out constantly. They show how quickly the disease and its side effects worsen. Clues include blood pressure, blood values for some proteins and electrolytes, and body weight.
In late stages, specialists examine the possibilities for renal replacement therapy individually. In the final stages, they are the only way out to prevent life-threatening urinary poisoning.
Important kidney values
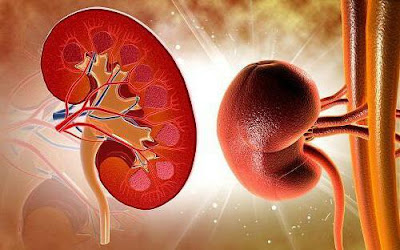
Kidneys filter the blood that comes to them through the renal arteries. They hold back substances that the body can still use, such as intact proteins and blood cells. Substances that have to be urinated, i.e. substances that are unnecessary for the body, and excess water are excreted as urine via the urinary tract.
- Glomerular filtration rate (GFR): When kidney performance decreases, the amount of cleaned blood drops below normal. The "clearance" decreases. The most important value for kidney performance is the glomerular filtration rate (GFR): the lower the GFR, the weaker the kidney function. It is usually given in milliliters per minute (ml/min). In healthy adults, GFR is between 95 and 120 mL/min. The value decreases with age. In people over 60 years of age, it is less than 90 ml/min. If the kidney function is disturbed, there are often proteins in the urine or, in the case of inflammation, blood cells. To determine GFR, patients typically collect their urine for 24 hours. The samples also show which blood components the kidneys can excrete and which cannot.
- Creatinine levels and creatinine clearance: One of the proteins that the kidneys remove completely from the body is creatinine. A rising creatinine level in the blood indicates that the organs are working less well. Healthy adults have creatinine levels of between 0.6 and 1.4 milligrams per deciliter (mg/dL). Creatinine clearance indicates how well the kidneys remove creatinine from the blood. Normal values are 75 to 160 ml/min. In the case of creatinine clearance, lower values indicate disorders.
Stages of chronic renal failure
The simplest system for grading chronic kidney failure is based only on GFR. It includes five stages, or sometimes just four. Then "Stage 1" or "Stage 5" is missing from the following list:- Stage 1 - GFR 90 mL/min or more: The kidneys are working normally. The levels of urinary substances in the blood are also normal. These people are healthy as long as they do not excrete too much protein (technical term: proteinuria) or there are no pathological changes in the kidneys in imaging procedures (e.g. ultrasound, computed tomography). Such anomalies tend to come to light by chance, for example during cardiovascular checks. Those affected usually have no symptoms. Therapies should prevent the disorder from progressing. Above all, this includes doing something about possible risk factors and causative diseases such as diabetes and high blood pressure. Regular measurements of the GFR show whether the condition is changing.
- Stage 2 – GFR 60 to 89 ml/min: The kidneys are still working so well that symptoms only occur in exceptional cases. Those affected are not necessarily considered to have kidney disease if there are no additional negative findings. In addition to blood tests, more precise kidney tests are needed to clarify the situation. Therapies should keep kidney function stable for as long as possible. Measures are also needed to counter additional adverse factors and illnesses.
- Stage 3 – GFR 30 to 59 ml/min: Symptoms are now often clearly noticeable. Affected people complain about symptoms that they themselves can only rarely attribute to kidney disease. The majority suffer from poor performance and fatigue. Blood tests show elevated levels of substances that are excreted in the urine, and blood pressure is usually also elevated. The risk of cardiovascular disease increases significantly. Doctors now have to adjust the doses of drugs that are excreted through the kidneys to the reduced performance of the kidneys. Otherwise, side effects may occur or existing ones may intensify.
- Stage 4 – GFR 15 to 29 ml/min: Kidney function continues to decline, which can lead to worsening and new symptoms. These include, for example, loss of appetite, nausea, vomiting, itching and pain. The body can retain fluid, edema often develops on the legs and face. The number of red blood cells and bone substance may decrease.
- Stage 5 – GFR below 15 ml/min: The kidney function is almost completely absent. Experts speak of terminal renal insufficiency or sometimes of kidney failure in the narrower sense. Measures must be taken quickly here so that the body does not become poisoned. Harmful substances that would otherwise be disposed of by the kidneys have to get out of the body in some other way. Renal replacement therapies/renal replacement procedures such as dialysis and kidney transplantation serve this purpose.
Lifestyle changes
As a rule, doctors and patients develop individual plans as to what drinking habits, diet and lifestyle should look like in the future. The plans are adapted to the condition of the kidneys. They address possible concomitant diseases and the high risk of cardiovascular disease in patients. You should also prevent infections as best you can.When it comes to nutrition, it is fundamentally important that it protects the kidneys. At the same time, however, there should be no states of deficiency. The salt and acid-base balance should also remain largely normal.
- Diet: Those affected should eat less protein. The kidneys have to filter out proteins in order not to retain them in the body. If you save on the amount of protein, you relieve the kidneys. On average, adults consume around 1.3 grams of protein per kilogram of body weight every day. In the case of chronic kidney failure, the amount should drop to 0.8 to 0.6 grams - depending on the stage and only before dialysis is required. Affected people should usually consume less meat and dairy products, but at the same time continue to eat enough calories. This is often difficult for them, for example because the recommended menu does not suit them or they are hardly hungry because of their illness. As soon as patients require dialysis, their protein requirements increase again. You now have to be more careful not to take in too much phosphate, which is often found in meat products. A lot of phosphate accelerates the breakdown of bone substance, which threatens in the late stages. Patients often have to reduce their intake of potassium.
- Amount to drink: How much liquid those affected should drink depends on their kidney performance. In the beginning, when the amount of urine is still normal, it means drinking a lot. Later, when the amount of urine decreases, the amount you drink must also decrease. The daily amount of liquid is very limited when dialysis is required and shortly before. Constant thirst can be very stressful for those affected. By stage 3, they should be able to self-monitor their hydration by weighing themselves each morning. Decreasing amounts of urine with simultaneous weight gain indicate fluid retention (technical term: edema). Those affected should reduce their fluid intake.
- Medications: As described in more detail under "Causal Treatment," certain medications can damage the kidneys and even cause kidney failure. Patients with chronic kidney failure should avoid appropriate medication.
- Other lifestyle: The patient's risk of cardiovascular problems is significantly increased. Therefore, they should adjust their lifestyle accordingly. It is very important to stop smoking. Regular exercise, normal weight, an even rhythm of life and other positive factors also have great advantages for those affected.
