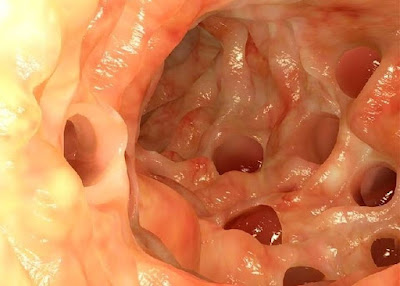
Diverticula, small protuberances in the intestinal mucosa, are usually harmless. However, when they become inflamed, it often leads to a dull ache in the lower left abdomen. This inflammation is called diverticulitis or – because of the location of the pain – also left appendicitis.
Intestinal diverticula are common, especially in older people. About a third of 60-year-olds have them, but most of those affected are symptom-free. The diverticula become inflamed in only about two out of ten sufferers. It is not yet clear why which diverticula become inflamed and when.
 |
| Diverticulitis |
Diverticulitis Causes, Risk Factors And Frequency
Why and with whom diverticula form is unclear, the study situation is not clear. Is diverticulosis a disease of civilization related to eating habits in western industrialized nations? Too little fiber, too little exercise, but constipation? Since low-fiber foods lead to a hard and firm stool and thus often to constipation, it was assumed that the pressure in the intestine could cause protuberances over time. This could also explain why diverticula are often found in older people in particular, whose connective tissue is weakening.
Recent studies turn these explanations on their head: lots of dietary fiber in food does not protect against diverticulosis, and neither constipation nor physical laziness have emerged as risk factors for the formation of diverticula.
However, what diet seems to have an effect on is whether the diverticula become inflamed and whether “silent” diverticulosis develops into diverticulitis. Both people who consume a lot of fiber and vegetarians are at much lower risk of developing diverticulitis than people who eat a low-fiber diet.
Risk factors
Risk factors for developing diverticulitis from diverticulosis and complications such as perforation and bleeding include:
- Medications such as non-steroidal anti-inflammatory drugs (eg, acetylsalicylic acid), oral steroids, opiate analgesics (opioids)
- Nutrition
- Smoking
Frequency
The frequency of intestinal diverticula forming increases with age. While only every 20th person in the 30 to 40 age group has these bowel protuberances, they occur in a third of the 60 year olds. For those over 80, the proportion increases to two-thirds. However, this does not mean that the diverticula become inflamed. This only applies to 12 to 25% of those affected.
Diverticulitis Symptoms
Do you have a dull pain in the lower left abdomen?
Do you suffer from intestinal problems such as constipation, bloating and diarrhea at the same time?
Such symptoms may indicate diverticulitis. Generally, diverticula are harmless whether someone has just one diverticula or multiple (diverticulosis). In eight out of ten people affected, the protuberances do not cause any symptoms (asymptomatic diverticulosis). However, if the diverticula become inflamed, the pain usually occurs on the left side. This is because most diverticula form in the descending part of the colon, where the bowel makes an S-curve (sigmoid colon, sigma) in the left abdomen.
Symptoms of diverticulitis can include:
- Uniform and dull abdominal pain in the left lower abdomen (left appendicitis, sigma diverticulitis), but also in the entire left abdominal area; rarely right
- Improvement of pain after defecation or after passing of intestinal gases
- Hardening in the abdomen that is painful to the touch or pressure
- Unpleasant, possibly painful urge to defecate
- Intestinal problems such as constipation, flatulence, diarrhea
- Pus, mucus, or blood in the stool
- Nausea and vomiting
- Fever and fatigue
- Atypical symptoms such as an increased urge to urinate or problems urinating if the inflammation has spread to the bladder
If the inflammation is limited to individual diverticula, doctors speak of peridiverticulitis. If it spreads to larger areas of the intestine, it is called pericolitis. Experts further divide diverticulitis into three stages.
- Stage 0: The affected person has diverticula, but they do not cause any symptoms.
- Stage I: When the diverticula are inflamed but the inflammation is limited to the intestinal wall, doctors speak of acute uncomplicated diverticulitis. Conservative treatment is possible, surgery can be avoided.
- Stage II: In acute complicated diverticulitis, the inflammation has spread through the intestinal wall (II a: extensive surrounding inflammation, II b: covered perforation, II c: free intestinal perforation). There may be other symptoms such as abscesses, fistulas, an intestinal blockage or a hole in the intestinal wall (perforation). In stage II, an operation is usually necessary to stop the progression of the disease.
- Stage III: Diverticulitis that keeps coming back is called chronically recurrent. The intestinal wall can be thickened, or the interior of the intestine is narrowed (stenosis). Tubular connections (fistulas) may also have formed between the intestines and other organs (bladder, vagina). Those affected experience recurring pain, constipation and possible discomfort in the adjacent organs.
Diverticulitis Treatment
The right therapy for diverticulitis depends on how severe the inflammation is and which parts of the intestine and surrounding area are affected. Acute, uncomplicated diverticular disease does not require any special therapy; fasting and drinking plenty of fluids usually help. When taking painkillers, it is advisable to avoid non-steroidal anti-inflammatory drugs such as acetylsalicylic acid, ibuprofen and diclofenac, as studies have shown that they increase the risk of diverticulitis. Painkillers such as paracetamol are considered to be better tolerated. According to current studies, antibiotics are of little help in acute uncomplicated diverticulitis.
When to the doctor?
If the pain in the lower abdomen is accompanied by fever and a general feeling of illness, it is advisable to consult a doctor. If you have blood in your stool, it makes sense to see a doctor.
A doctor will talk to the person about their medical history (anamnesis) before treatment. What complaints does the person concerned have? Are the symptoms appearing for the first time or are they recurring? It is also important for the physician to find out whether diverticula have already been diagnosed in an earlier examination.
During the physical examination, the doctor may be able to feel the "roller" in the lower left abdomen that is typical of diverticulitis. Maybe he will also do a palpation of the anus. A blood test can be used to determine inflammation values such as white blood cells (leukocytes), blood cell lowering speed (ESR) and increased C‑reactive protein (CRP). Ultrasound, computer tomography or magnetic resonance imaging provide information about the size and position of the diverticula. A standing X-ray shows whether air has built up in the abdomen, indicating ruptured diverticula.
If those affected have severe pain and fever, the doctor will advise inpatient treatment in the hospital. Those affected are often not allowed to eat any solid food. Depending on the therapy, they are given liquid food or are attached to an infusion for intravenous nutrition. If necessary, they will also receive antibiotics. If the treatment is successful without surgery and the symptoms improve, build-up with normal food takes place after two to three days.
If the therapy does not respond or if there are complications such as an intestinal perforation, a surgeon will remove the damaged section of intestine in an operation. The procedure can be postponed until the acute flare-up of inflammation has subsided. Sometimes it is also necessary to operate on an emergency basis, for example when diverticula have ruptured. Surgery can be done openly through an abdominal incision or through laparoscopy. With the latter, only an endoscope is inserted into the abdominal cavity.
Prevention
Diet doesn't seem to have much of an impact on getting diverticula. However, whether the harmless diverticula develop into an unpleasant diverticulitis, a high-fiber diet with lots of roughage can change that.
- A high-fiber diet means eating lots of fruit, vegetables and whole grain products because they are rich in fiber and fibre.
- Do not use products that have been ground too coarsely, as food components that are too hard and sharp can injure the diverticula.
- If you don't manage to eat enough fiber-rich foods, you can enrich your food with more fiber with wheat bran or oat bran and ground flaxseed.
- Drink plenty of fluids: It is recommended to consume two to two and a half liters of fluids per day.
- Exercise keeps the gut going. Endurance sports such as hiking, running and swimming are particularly suitable.
